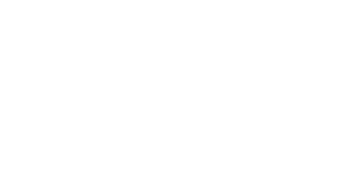
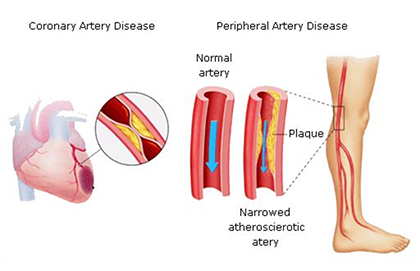
Peripheral artery disease (also called peripheral arterial disease) is a common circulatory problem in which narrowed arteries reduce blood flow to your limbs.
When you develop peripheral artery disease (PAD), your extremities — usually your legs — don’t receive enough blood flow to keep up with demand. This causes symptoms, most notably leg pain when walking (intermittent claudication).
Peripheral artery disease is also likely to be a sign of a more widespread accumulation of fatty deposits in your arteries (atherosclerosis). This condition may be reducing blood flow to your heart and brain, as well as your legs.
Often, you can successfully treat peripheral artery disease by quitting tobacco, exercising and eating a healthy diet.